The Malaria-Sickle Cell Connection
April 19, 2017
A recent study has found a connection between hereditary sickle cell disease and malaria, a dangerous parasitic disease transmitted by mosquitoes. The study determined that genetic mutation responsible for sickle cell disease, a serious blood disorder, rapidly spread through human populations in Africa more than 40,000 years ago mainly because it provides protection from malaria. Genetic scientists used computer-based models to understand the conditions that spread the sickle cell mutation among certain human populations. The scientists learned that this mutation was among the most important factors affecting survival over the last 40,000 years for people living in malaria-affected regions. The study’s results were published on March 10, 2017, in the scientific journal PLOS Genetics.
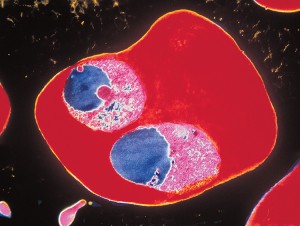
A new study has shown that people carrying the sickling gene that can cause sickle cell disease have a higher natural resistance to malaria parasites, shown here in pink and blue. Credit: © CNRI/SPL from Photo Researchers
Sickle cell disease, also called sickle cell anemia, is a hereditary blood disease. In the United States, it occurs chiefly among African Americans. It also affects other groups, including people of Central African, Mediterranean, Middle Eastern, and South Asian origin. Sickle cell patients have an abnormal type of hemoglobin, the oxygen-carrying protein that gives red blood cells their color. This abnormal protein, called sickle hemoglobin, or hemoglobin S, forms crystals in red blood cells. This causes the normally round red blood cells to change into twisted, rigid sickle-shaped forms. The sickle cells can get trapped and block the normal flow of blood through blood vessels. This disruption of blood flow causes periodic crises (attacks of severe pain and fever) and related problems including strokes, lung or kidney damage, and sudden death.
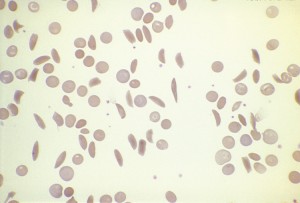
This magnified blood sample shows the red blood cells of a person with sickle cell anemia. Normal red blood cells appear round in the image. But, abnormal, sickle hemoglobin causes many red blood cells to change into twisted, rigid sickle forms. Credit: © Bruce Coleman Inc./Alamy Images
Scientists know that harmful mutations, such as the one responsible for the abnormal sickle hemoglobin, should become less common in populations over time because of the process of natural selection. Natural selection sorts out these random changes according to their value in enhancing the individual’s reproduction and survival. In the past, people with sickle cell disease rarely survived long enough to have children. Today, modern medicine has improved the health and life span of people with the condition.
Scientists have lately learned that carriers of the sickling gene—that is, people who have only one copy of the mutated gene instead of two—not only have normal blood cells, but they also have a higher natural resistance than noncarriers to malaria. Sickle cell anemia is a rare disorder, but it occurs most often among populations that live in areas threatened by malaria. Thus, the sickling gene—despite its negative effects for some—represented an important advantage for other people in these tropical and subtropical regions. The new research shows that the sickle cell mutation had a rapid and dramatic effect in shaping the genetic makeup of certain human populations in the past. Such dramatic changes are also possible in the future, as human populations continue to adapt to a constantly changing global environment.


